Track 1: Palliative and Hospice Care:
When treatment isn't typical, palliative and hospice care is the active, expert, and sensitive support of people dealing with a real, reformist sickness. The goal of hospice and palliative care is to support and enhance personal fulfilment for persons who are nearing the end of their lives and their families. Through an interdisciplinary group of professionals including experts orderlies social workers, home consideration nurses, home helpers, Hospice staff and chips in, and various controls, this provides social, enthusiastic, and profound aid to individuals and families. With Hospice benefit, the objective is to assist patients in reducing their discomfort and enduring while in a critical situation. However, palliative care is a method that focuses on the personal fulfilment of patients with real illness; it corrects the path by the prevention of suffering and assistance with it through early detection of evidence, excellent evaluation and treatment of suffering, physical, psychosocial, and other concerns, effective providing support for the family at times of loss
Track 2: Palliative Care Nursing:
Control of manifestations, while remaining delicate to individual, social and strict characteristics, accepts and rehearses. The job of Nursing in palliative consideration is to give alleviation from act Palliative Care Nursing helps us in achieving life past treatment through alleviation from affliction dual side effects
Track 3: Hospice and Palliative Medicine:
In the United States, hospice and palliative medicine is a recognised specialisation of medicine that focuses on end-of-life care, indication the board, and pain relief. The American Board of Medical Specialties made a formal assessment of hospice and palliative care in 2006. This authority has dominance in the evaluation of patients with cutting-edge illness and catastrophic injury the assistance of distressing side effects, the coordination of interdisciplinary patient and family-engaged thought in organised settings, the use of particular thought systems like hospice, the organisation of the rapidly approaching-death patient, and the moral and legal dynamics in end-of-life care
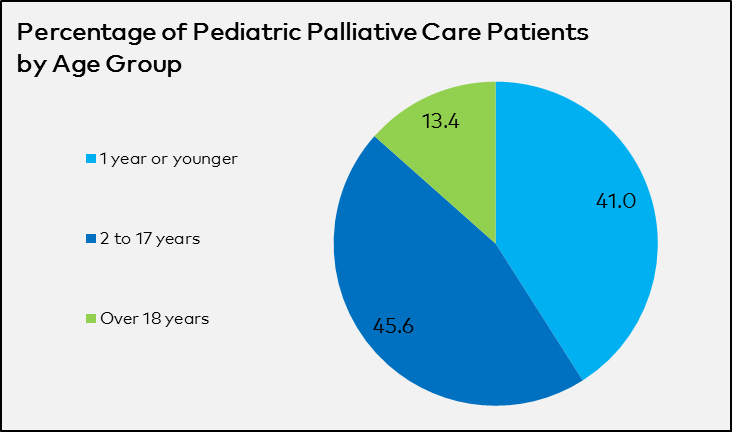
Track 4: Pediatric and Neonatal Palliative Cares:
Palliative care for children and newborns is a special clinical concern for those with life-threatening medical diseases, such as genetic disorders, prematurity cancer, neurological abnormalities heart and lung conditions, and more Teenagers' palliative care includes supporting the family as well as giving fiercely entire attention to the child's body, mind, and soul. The goal is to improve both the family's and the child's quality of life. Additionally, child brain research aids in improving paediatric care. A group of experts medical professionals and other professionals offer paediatric and neonatal palliative consideration as an additional level of assistance. It gives the family and child the ability to move forward step by step for the time being
Track 5: Palliative Care for Psychiatry & Neurological Disorders:
A method of caring for patients and their families who are dealing with progressive and chronic illnesses, palliative care focuses on easing symptoms brought on by real symptoms, psychosocial problems, and severe distress. A common perspective between psychiatry and palliative care is that both fields have developed significantly from internal medicine, are based on the bio psychosocial paradigm and frequently collaborate with other specialists. Traditional forms of palliative care, according to the analyst, don't adequately address the unique needs of patients and their families who are dealing with a neurologic ending. Most developed nations have seen a significant increase in the last twenty years in collaboration between the fields of psychiatry and palliative consideration, which is frequently taught under the heading of palliative consideration
Track 6: Palliative Care and End of life Care:
End-of-life care is assistance for those who have been living for a while or for extended periods of time. Palliative contemplation is combined with end-of-life care. If you have a disease that can't be cured, palliative care helps you feel as comfortable as possible given the circumstances by addressing your annoyance and other distressing symptoms. It also includes assistance for your family or caregivers and you in the form of mental, social, and paranormal support. Since it handles you "all in all," rather than just your condition or side effects, this approach is known as a comprehensive methodology. You can receive palliative care early in your illness while still receiving other types of care; it's not exclusively for people who are nearing the end of their lives
Track 7: Gerontology and Geriatric Palliative Care:
The medical area of geriatrics deals with the care of elderly people. Geriatrics focused doctors assist older patients with the physical changes that their bodies undergo as they age. Gerontology is the rational study of maturing as a cycle of the physical, social, and psychological kinds. Reviewers usually reference academic authorities from other, diverse domains. However, there are some fundamental differences between gerontology and geriatrics in terms of how they approach the elderly and what they ultimately contribute to the field of senior review and care. For older patients, the main challenges may be a sudden shift in mental state, excruciating pain, shady symptoms, declining health, dehydration, anorexia, and odd clinical reactions
Track 8: Pain & Symptom Management in Palliative Care:
A very evident and upsetting side effect in individuals introducing toward the end of life is agony. Despite this, many people who are suffering from a terminal illness fear suffering because they believe that doing so would result in terrible unintended consequences. Agony's overall impact is increased by fear of punishment. Talking about your annoyance and your feelings of fear in respect to suffering is crucial. Patients who suffer from neurological disorders that are terminal, such as ALS or stroke, may also feel excruciating pain. The majority of agonies can be lowered or controlled. Assessing and observing all facets of suffering is necessary for controlling it and keeping it there. These are the core skills of medical assistants and professionals in palliative care
Track 9: Palliative Care in Emergency Medicine & Trauma:
Genuine symptoms like ongoing pain and others are basically brought on by injury. In the United States, injury continues to be a major source of misery and death. Palliative care has the distinction of providing treatment for patients who have actual, serious, or life-limiting illnesses or injuries, regardless of their stage of illness or stage of treatment. Palliative care aims to lessen or lessen the long-lasting executive agony side effects of the executives, and in addition, to provide further aid with dynamic. The combination of palliative and injury care can aid and assist patients and families through distressing, frequently ground-breaking circumstances while paying little attention to a clear result
Track 10: Palliative Care in Oncology:
Malignant growth frequently results in reactions, as does its treatment. Helping someone with their symptoms and unintended consequences is an essential part of disease treatment. Palliative care, strong care, or manifestation executives are terms used to describe this type of treatment. Palliative care offers expert therapy and provides care for symptoms, as well as care for their side effects and emotional problems. In the midst of a patient's involvement with disease, palliative consideration is given. It should begin with decision-making and continue through treatment, aftercare, and death. Malignancy symptoms may include pain, illness, regurgitation, fatigue, sadness, clogging, the runs, disarray, or exhaustion. Specialists in palliative care have the expertise to decode complex clinical insights and can help you understand
Track 11: Palliative Care in Genetic Disorders:
Additionally, complex or polygenic hereditary issues may be multifactorial and caused by one or many quality anomalies. There is currently minimal research focusing on concerns related to end-of-life care for individuals with genetic conditions, and there is a lack of a suitable model of care to pursue for end-of-life therapy or cessation of treatment. Different hereditary infection sufferers now have longer lifespans because to innovative developments. The hospice initiative to help those with inherited conditions is where the struggle of life programme got its start. A medical professional assists the brain-damaged in reaping the maximum amount of benefits from life
Track 12: Alternative Healthcare in Palliative Care:
In order to revamp palliative or end-of-life care, complementary medicines are turning up logically applied in the middle of a condition's final phases. These seek to ease the patient's suffering and the terror associated with the mysterious, as well as its alleviation and departure. These medications combine directed relaxation and symbolism, music therapy, helping touch, and fragrance-based treatment to restore the body/mind balance. They are believed to be effective in reducing muscle tension, reducing the patient's need for pain medication, improving sleep quality, and reducing stress
Track 13: Palliative Care in Rehabilitation and Occupational Medicine:
Enhancing personal contentment is a key component of rehabilitation medicine. Patients commonly encounter testing mental distress as a result of their illness and the therapy while receiving determination and treatment. Rehabilitative consideration identifies methods to treat common obstacles to goal-achievement, such as fatigue, tension, and discouragement. By identifying patients' vital life occupations and activities (or "occupations") and removing barriers to carrying them out, word-related treatments play a significant role in palliative and hospice care groups. They focus on what is typically basic for that person to complete, the open resources and genuinely stable organizations, and the situations where the patients demand and can receive both physical and psychosocial/social prosperity needs, which is different from other medical care
Track 14: Palliative Care and Spiritual Care:
You can think of profound care as something that notices and responds to human soul. Additionally, Otherworldly Care covers the universal human needs for admiration, relatedness, expectancy, regard, and nobility. Strict emotions and behaviors may be present in otherworldliness. A crucial area of palliative thought is profound consideration, which focuses on the needs of the complete person and their family. The supernatural has a big role in the human experience. Every great regard and virtue—such as consideration, fairness, empathy, compassion, regard, pardoning, trustworthiness, cherishing, concern toward patients, and respect for nature—has a spirit and a purpose that are inspired by this principle. Deep Care is a planned partnership that embraces focused contemplation and excludes any assumptions about personal judgement or life direction
Track 15: Health Issues in Palliative Care:
Numerous problems can be addressed by palliative care. The mental and physical repercussions of illness might vary, and considerations including age, social standing, and personal emotional support networks influence the type of thought that is necessary. A comprehensive view of palliative care takes into account practical problems, passionate and adjusting requirements, and physical necessities